The December 2017 Sixty Second Survey on Dupuytren Triggers was the most data-packed survey to date. This survey focused on a simple-sounding question: is the onset of Dupuytren disease triggered by an external event such as injury, physical activity, medication, or emotional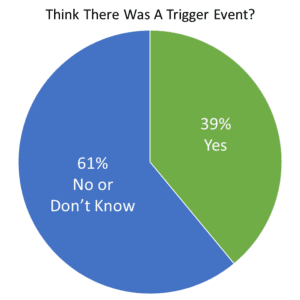 stress? Almost 40 percent of those taking the survey believed that some event triggered their first signs of Dupuytren disease. What did the survey show? Let’s dig in.
stress? Almost 40 percent of those taking the survey believed that some event triggered their first signs of Dupuytren disease. What did the survey show? Let’s dig in.
Study design
One way to test whether events trigger Dupuytren would be to survey people with and without trigger events and see who develops Dupuytren and who doesn’t. This isn’t practical. This study took the opposite approach: survey people with Dupuytren and see how many remember trigger events. The challenge with this is not knowing whether 40 percent is high or low for the general population. For example, a recent Harvard study found 49 percent of the general population reported a major stressful event or experience within the last year (https://media.npr.org/documents/2014/july/npr_rwfj_harvard_stress_poll.pdf). Percentages for other trigger categories in the general population are unknown. What to do? Knowing that Dupuytren is different in different people, this study correlated trigger events with different aspects of Dupuytren, such as the age of onset, number of bent fingers, nodules, and risk factors for aggressive Dupuytren disease.
Study Demographics
The first step is sorting the types of Dupuytren in people who took the survey. 845 Dupuytren sufferers took the survey. It’s a well-rounded sample: half men, half women; half with Dupuytren in the family, half without. 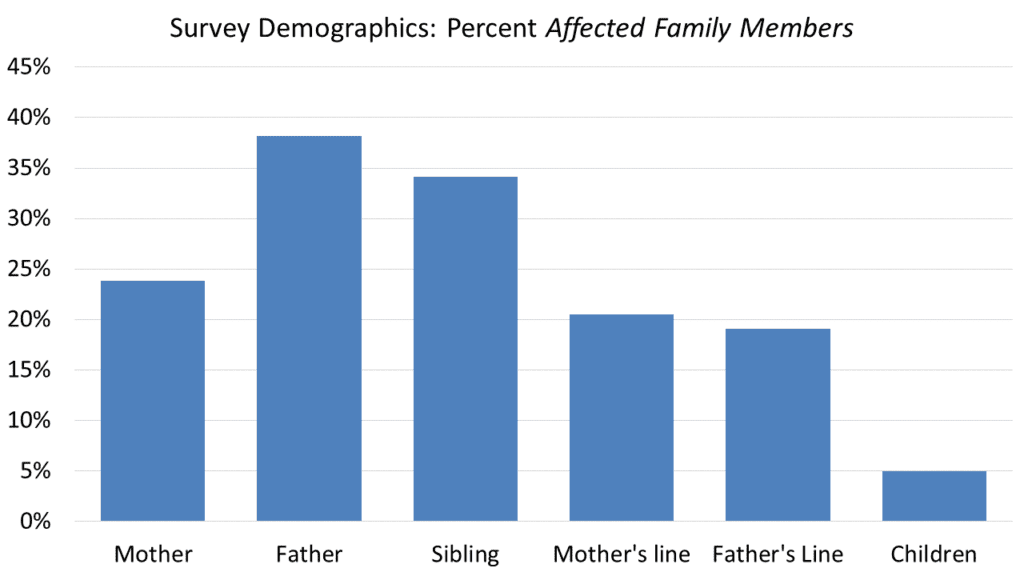 Both hands were affected in two-thirds; one-third had only one hand involved. Over four out of five reported Dupuytren nodules, fingers bent by Dupuytren contracture, or both. Six out of ten reported one or more Dupuytren spectrum disorders: knuckle pads, Ledderhose disease, frozen shoulder, or Peyronie disease.
Both hands were affected in two-thirds; one-third had only one hand involved. Over four out of five reported Dupuytren nodules, fingers bent by Dupuytren contracture, or both. Six out of ten reported one or more Dupuytren spectrum disorders: knuckle pads, Ledderhose disease, frozen shoulder, or Peyronie disease.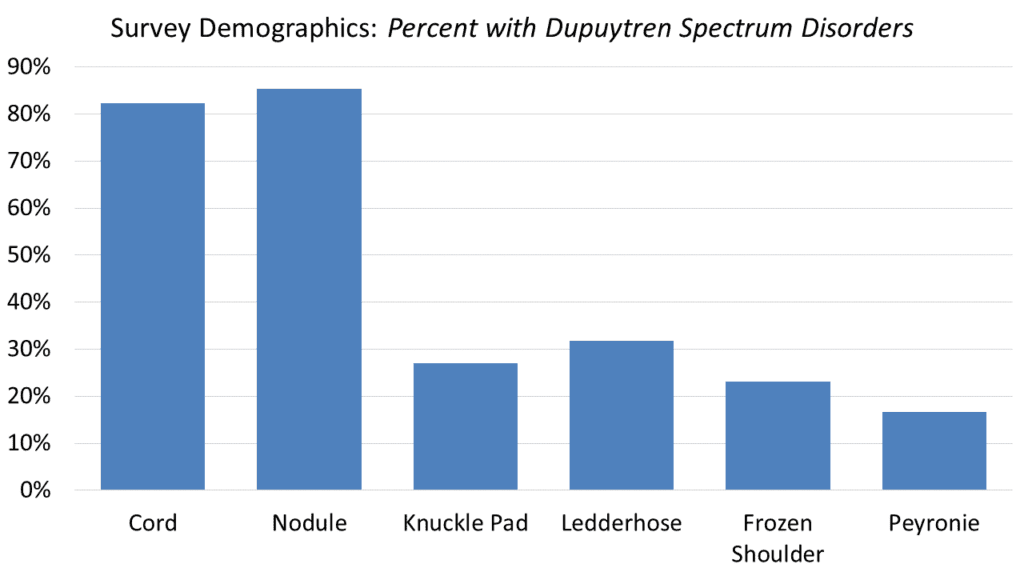 There were gender differences in Dupuytren spectrum disorders similar to prior reports. One out of six men reported Peyronie disease. One of three women gave a history of frozen shoulder – twice the rate of men, and statistically significant. There were no gender differences in the reported percentages of Ledderhose or knuckle pads.
There were gender differences in Dupuytren spectrum disorders similar to prior reports. One out of six men reported Peyronie disease. One of three women gave a history of frozen shoulder – twice the rate of men, and statistically significant. There were no gender differences in the reported percentages of Ledderhose or knuckle pads.
Age of first signs of Dupuytren is thought to correlate with Dupuytren aggressiveness. The average age of onset is typically reported as 10 to 15 years younger for men than women. In this survey, the age midpoint (half younger, half older) was 50 for men and 55 for women. This may mean the women taking this study had aggressive disease compared to the average.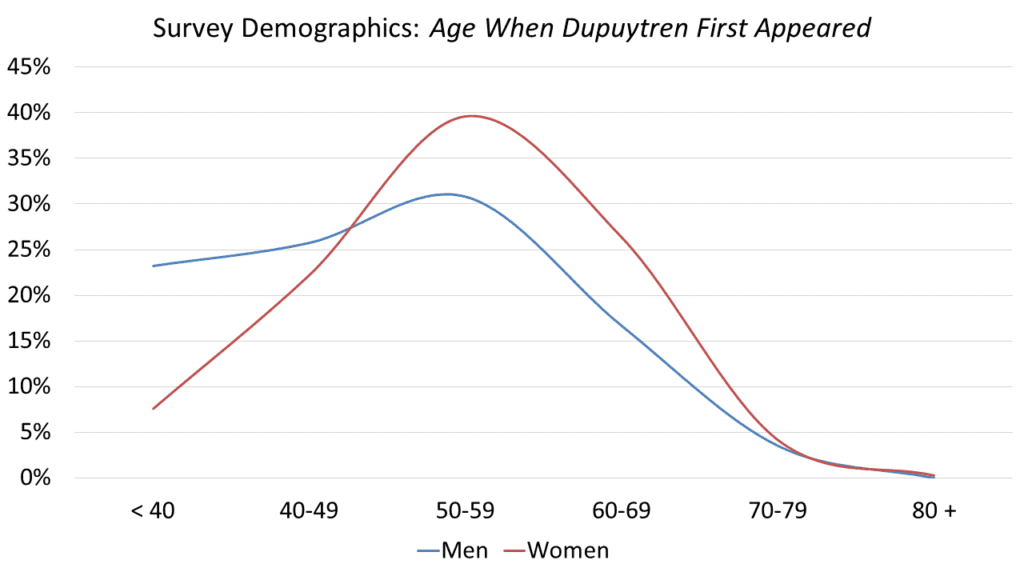 Trigger categories
Trigger categories
Triggers were defined as events within a year before to the first evidence of Dupuytren disease. Triggers were grouped into four categories: Injury (accidental: broken wrist, cut needing stitches, dislocated finger, etc., surgical: surgery for carpal tunnel, trigger finger, hand arthritis, etc.), Activity (unusually strenuous activity: new job duty, home remodeling project, new sport or exercise routine, etc.), Medical (new medicine or medical treatment), Stress (personal life event: divorce, personal health crisis, death of a loved one, house move, living through a natural disaster, etc.).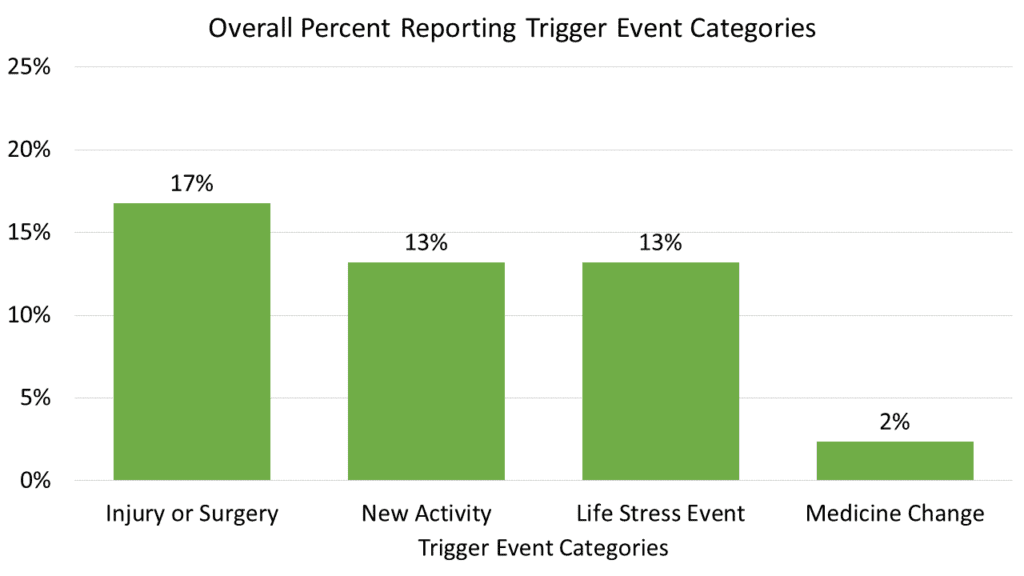 Statistical significance
Statistical significance
Just because numbers look different on a chart doesn’t prove they aren’t due to random chance. The answer to this question is important, and enough people participated that it was possible to perform formal analysis for statistical significance. The Chi-squared test was used and only results with greater than 95% likelihood of being true are shown below.
What didn’t correlate?
Diathesis factors. Dupuytren diathesis factors include a family history of Dupuytren, onset younger than 50, knuckle pads, Ledderhose disease, both hands involved, or more than two digits involved. Prior studies have concluded that people with several diathesis factors are more likely to have re-contracture after Dupuytren surgery. There was no statistical difference in the percent of people with diathesis factors versus no diathesis factors reporting any category of trigger events.
Dupuytren spectrum disorders. Spectrum disorders are associated with Dupuytren but haven’t been found to predict re-contracture after surgery. These include frozen shoulder, Peyronie disease, and psoriasis. There was no statistical difference in the percent of people with versus without Dupuytren spectrum disorders reporting any category of trigger events.
What did correlate?
Overall trigger events
A higher percentage of people who never had finger contractures reported trigger events than those who had developed contractures.
A higher percentage of people who ever had only one bent finger reported trigger events than those with more than two finger contractures.
A higher percentage of people who never had finger nodules reported trigger events than those who had finger nodules.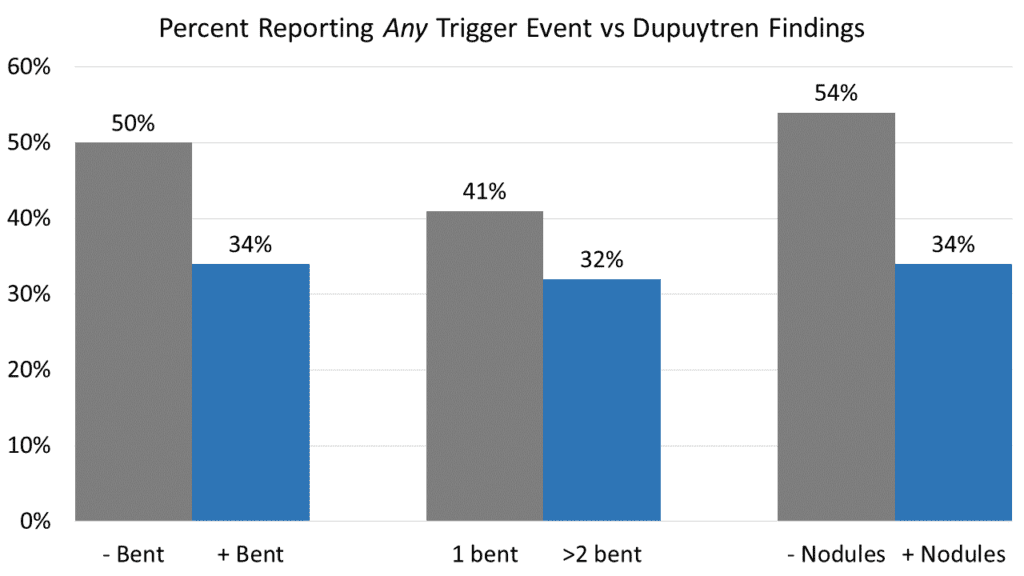
Injury trigger events (same-hand trauma or surgery)
A higher percentage of people who ever had only one bent finger reported injury trigger events than those with more than two finger contractures (more aggressive disease).
A higher percentage of people who never had finger nodules reported injury trigger events than those who had finger nodules.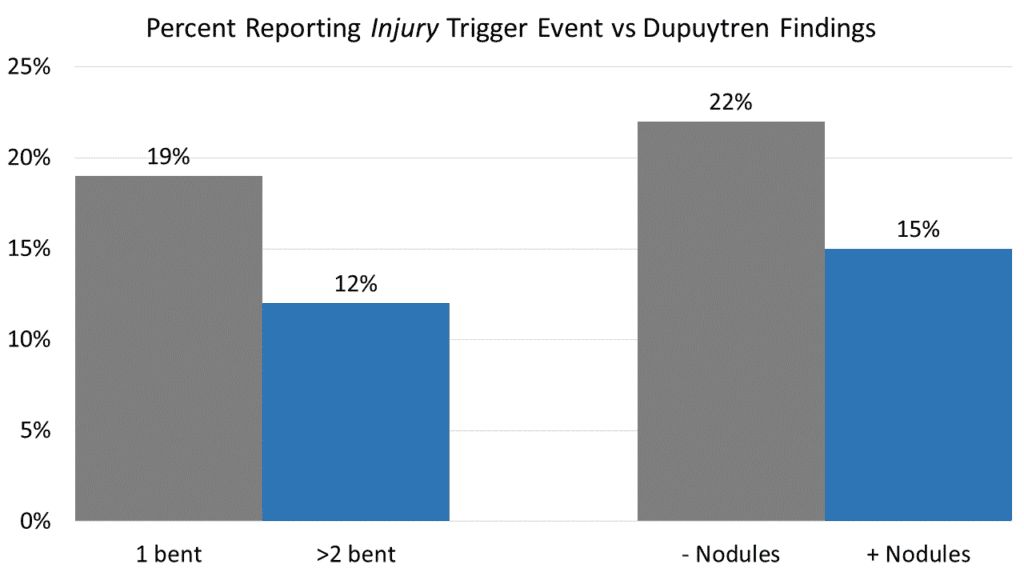
Stressful life events
Almost twice as many people who never had finger contractures reported stress trigger events than those who had developed contractures.
New strenuous manual activities
Almost twice as many people who never had finger nodules reported activity trigger events than those who had nodules.
Changes in medicine or medical diagnosis
Although the numbers were small, a higher percentage of people who were 50 or older when diagnosed reported a non-Dupuytren medical event than those who were younger than 50 when the first signs of Dupuytren appeared.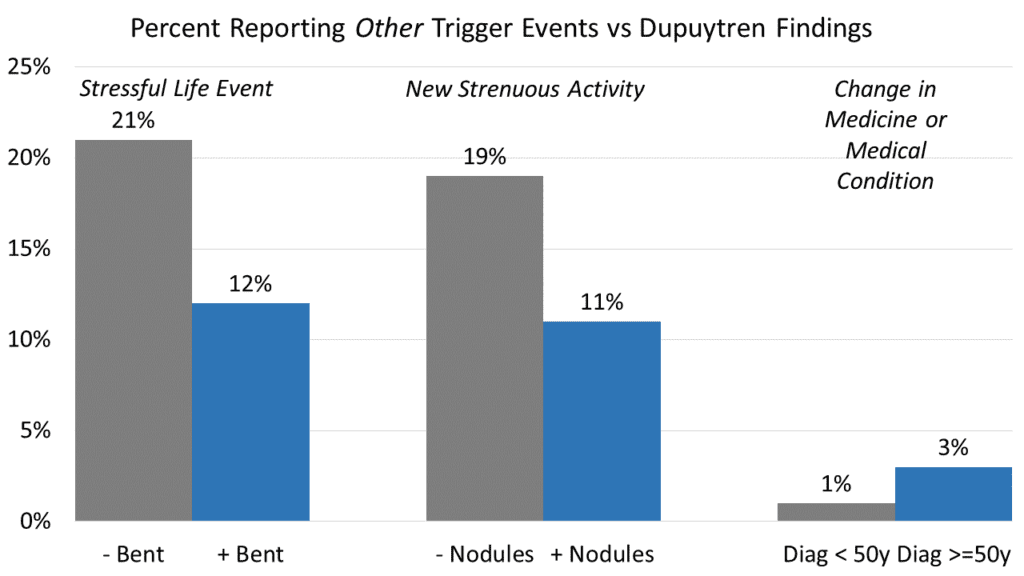 Trigger events in people with less severe Dupuytren biology
Trigger events in people with less severe Dupuytren biology
Trigger events were more common in people with nodules but no contracture than in people with nodules and contracted fingers. This difference was statistically significant for events in general, for stress triggers and to a lesser degree (91% rather than 95% probability) for injury triggers.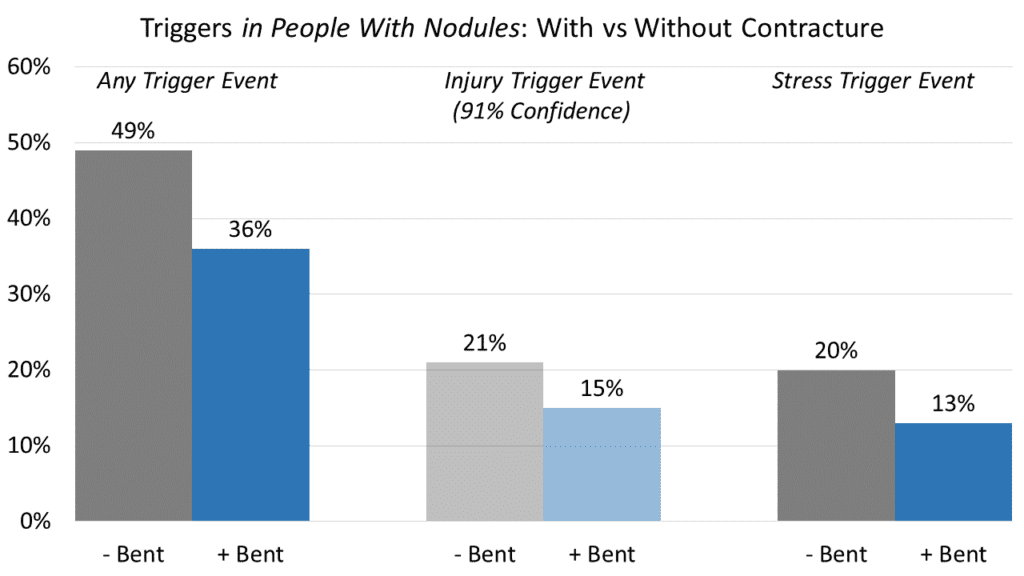 What does this mean?
What does this mean?
Trigger events do influence the onset of Dupuytren disease. Based on anecdotal experience, it’s commonly believed that trigger events play a role in the first appearance of Dupuytren. This study confirms there is a relationship – but it’s complex and only for a subset of Dupuytren patients.
Trigger-associated Dupuytren is less likely to be severe. People reporting Dupuytren trigger events were less likely to have nodules, less likely to have contractures, and if they did have contractures less likely to have contractures of many fingers. This is consistent with published descriptions of palm changes which look like early Dupuytren disease but rarely progress to contracture, particularly after a hand injury, hand surgery, diabetes, and long-term medications such as barbiturates. This picture has been referred to as pseudo-Dupuytren, non-Dupuytren disease, and traumatic palmar fasciitis. It’s hard to sort out because there’s no Dupuytren blood test to measure Dupuytren severity – but this is a step along the path to an answer.
It’s not black and white. Trigger events are common. Everyone – people with mild, severe, and no Dupuytren risk experience trigger events on an ongoing basis. If Dupuytren follows a trigger, the trigger is more likely to be remembered; if not, more likely to be forgotten. It is complicated and the relationship to diathesis remains unknown. The important point is that this study showed that triggers do impact Dupuytren onset and that the overall outlook may be better for those who believe that something triggered their Dupuytren disease.
Thanks very much to everyone who participated in this survey. Your participation is the ultimate resource to better understand the complex world of Dupuytren.






